A 60 year old male patient came to general medicine OPD with the chief complaints of back pain and difficulty in breathing while walking
GENERAL MEDICINE E-BLOG
The patient’s consent was taken verbally prior to history taking and examination of his/her condition.
A 60 year old married male farmer from Gundala village came to general medicine OPD with the chief complaints of backpain from neck to hip and difficulty in breathing while physical activity
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic 6 months ago
6 months ago he had abrupt onset of dragging type of pain in the cervical to sacral region of back due to which he was not able to walk properly and his daily activities were restricted.
He also complains of dyspnea on exertion which started abruptly from the time of onset of pain.
He didn't have any associated headache but complains of 1 episode of projectile vomiting which contained food contents white in colour and was non bile stain and non blood stained. He also complained of decreased appetite from the onset of pain.
All of his symptoms were subsided on admission into hospital, where he had undergone surgery and continues to undergo dialysis. Neck pain was associated with stiffness which increased in the evening time and relieved on sleeping and refractory to medication.
He complains of appearance of white colored pruritic spots on both upper limbs and back which were found to be bleeding on scratching.
HISTORY OF PAST ILLNESS
He was diagnosed with diabetes mellitus and hypertension after admission into hospital and was regularly using medication.
He had history of surgery after admission .
No other significant past history.
FAMILY HISTORY
No significant family history.
PERSONAL HISTORY
Mixed diet
Decreased appetite which was improved on hospital stay
Inadequate sleep
Loose stools which are blackish in color and non mucoid seen after starting medication.
Occasional burning micturition.
No allergies
Smoking - beedi consumption half pack ( 7-8 no.) Per day since 2 years
Alcohol- 60 ml of whisky and a bottle of toddy per day since 30 years
GENERAL EXAMINATION
Physical examination
Patient was conscious coherent and cooperative
No pallor
No icterus
No cyanosis
No clubbing of fingers
No lymphadenopathy
Grade 1 of pedal edema
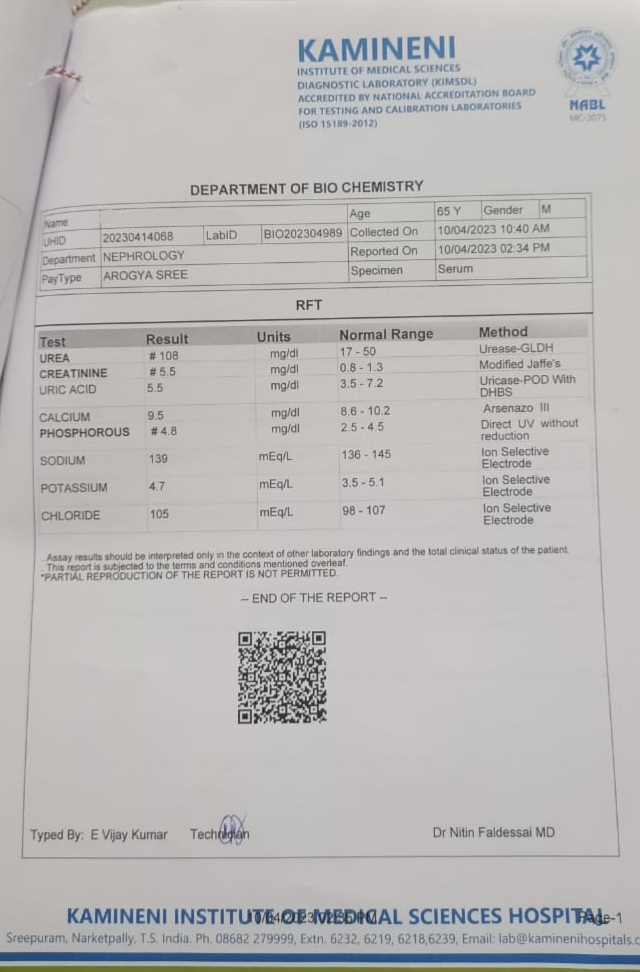
LABORATORY INVESTIGATIONS
Renal function tests
Serum Iron