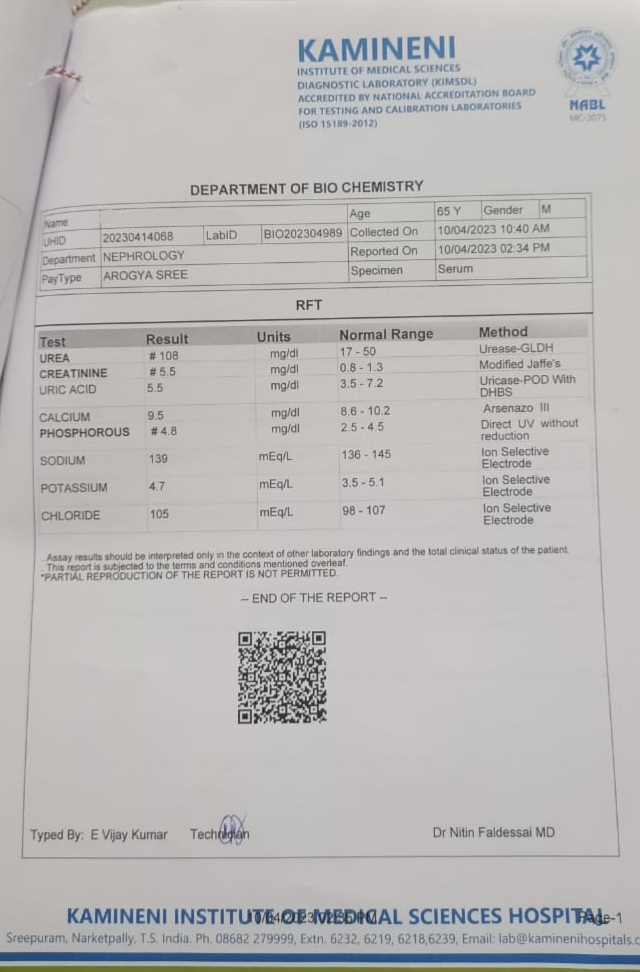
A 65 year old patient came to general medicine OPD with the chief complaints of swelling allover the body

GENERAL MEDICINE E-BLOG Hi, I am M. Sohith Mahadeva Reddy of 5th semester .This is an online E logbook to discuss our patient’s de-identified health data shared after taking his/her/guardian’s consent. This also reflects our patient centered online learning portfolio. The patient’s consent was taken verbally prior to history taking and examination of his/her condition. A 65 year old female housewife from Adaguduru mandal came to General Medicine OPD with chief complaints of swelling in the legs, abdomen, hands and facial puffiness since 1 week. HISTORY OF PRESENTING ILLNESS She was apparently assymptomatic 1 week ago. Then she developed sudden onset of generalized edema which was moderate in the beginning and gradually increased in the evening. It was associated with dypsnoea on exertion. It is not associated with pain, rise in temperature, nausea, vomiting and diarrhoea. She was taken to Suryapet hospital where she received medication which showed slight improvement and she came ...